7 Day Meal Plan for Pancreatitis: Managing Chronic Pancreatitis Through Nutrition
Managing pancreatitis through diet doesn't have to be overwhelming. A well-structured 7 day meal plan for pancreatitis can significantly reduce symptoms and improve your quality of life. This comprehensive guide provides a complete week of low-fat, pancreas-friendly meals designed specifically for chronic pancreatitis management.
Key highlights of this meal plan:
- 21 complete meals plus snacks (less than 35g fat daily)
- Evidence-based food choices that reduce pancreatic stress
- Practical cooking tips and meal prep strategies
- Expert-approved nutrition guidelines from 2024-2025 research
Whether you're newly diagnosed or looking to optimize your current diet, this 7 day meal plan for chronic pancreatitis offers the structure and variety you need to eat well while managing your condition effectively.
When I first received my chronic pancreatitis diagnosis three years ago, I felt overwhelmed by the dietary restrictions and conflicting information online. The thought of completely restructuring my relationship with food seemed daunting, especially when dealing with persistent abdominal pain and digestive issues. However, after working closely with nutritionists and experimenting with various meal plans, I've discovered that a well-structured 7 day meal plan for pancreatitis can dramatically improve symptoms and quality of life.
Living with chronic pancreatitis means your pancreas struggles to produce the enzymes necessary for proper digestion, particularly fat digestion. This condition affects approximately 50 out of every 100,000 people, yet finding practical, day-to-day meal planning guidance remains challenging. That's why I've created this comprehensive guide to help you navigate the complex world of pancreatitis nutrition with confidence and clarity.
Understanding Pancreatitis and Its Nutritional Challenges
Pancreatitis occurs when digestive enzymes become activated while still in the pancreas, essentially causing the organ to digest itself. This condition can affect your body's ability to absorb fat, causing oily bowel movements and vitamin deficiencies, especially vitamins A, D, E, and K. For those dealing with chronic pancreatitis, these challenges become long-term dietary considerations that require careful management.
The pancreas serves dual roles in your digestive system: producing insulin to regulate blood sugar and creating enzymes to break down fats, proteins, and carbohydrates. When pancreatitis damages these functions, your body struggles to process certain nutrients effectively, making strategic meal planning essential for symptom management and nutritional adequacy.
The Science Behind Pancreatitis Nutrition
Chronic pancreatitis represents chronic inflammation of the pancreatic gland with development of fibrosis, which progressively impairs the organ's ability to function normally. This inflammatory process creates a cascade of digestive challenges that directly impact how your body processes food.
Recent research has shown that chronic pancreatitis can cause poor absorption of nutrients, especially the fat-soluble vitamins A, D, E, and K. This malabsorption occurs because damaged pancreatic tissue cannot produce adequate amounts of lipase, the enzyme responsible for breaking down dietary fats.
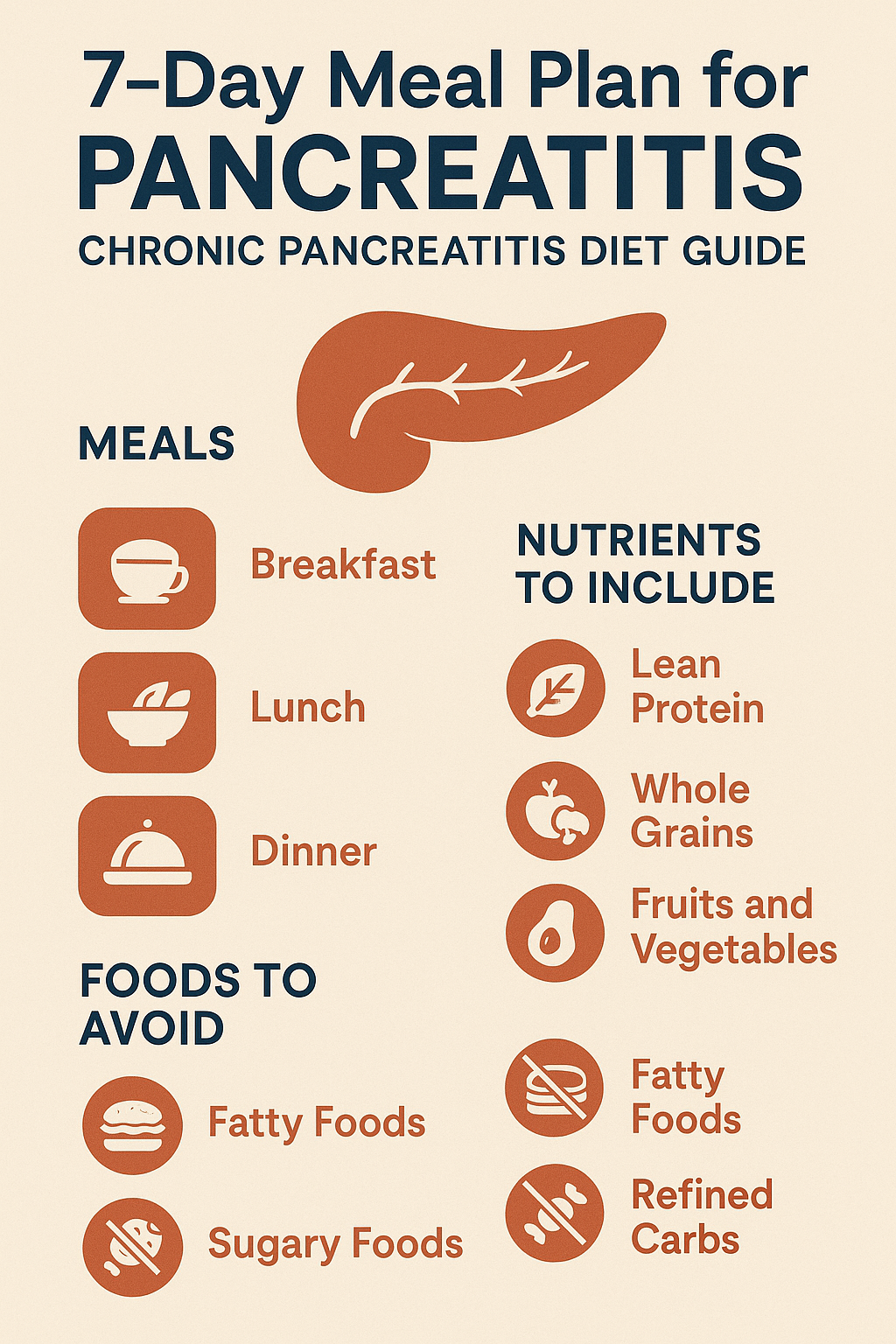
Essential Dietary Principles for Pancreatitis Management
Creating an effective 7 day meal plan for chronic pancreatitis requires understanding several key nutritional principles. These guidelines form the foundation of successful symptom management and long-term health maintenance.
Low-Fat Diet Strategy
The cornerstone of pancreatitis nutrition involves significantly reducing fat intake. Daily fat consumption should not be concentrated in one meal but spread throughout the day in possibly 4-6 small meals. This approach prevents overwhelming your compromised pancreas with large amounts of fat that it cannot adequately process.
Most healthcare providers recommend limiting fat intake to 20-30 grams per day during acute flare-ups, gradually increasing to 30-40 grams daily during stable periods. However, these numbers should always be individualized based on your specific condition severity and tolerance levels.
Frequent, Small Meals
Traditional three-meal-a-day eating patterns often prove too challenging for people with pancreatitis. Consider switching from three larger meals a day to three smaller meals with at least one snack. This eating pattern, often called grazing, allows your pancreas to work more efficiently by processing smaller amounts of food at regular intervals.
I've found that eating every 2-3 hours helps maintain stable blood sugar levels while preventing the digestive overwhelm that can trigger painful symptoms. This approach also ensures consistent nutrient absorption throughout the day.
Avoiding Problematic Foods
Certain foods consistently trigger symptoms in people with pancreatitis and should be eliminated or severely limited. Registered dietitians recommend that people with chronic pancreatitis limit their intake of refined carbohydrates such as white bread, sugary snacks, and sweetened drinks such as soda.
High-fat foods pose the greatest challenge for pancreatitis management. Avoid high-fat foods such as croissants, scones, biscuits, waffles, doughnuts, muffins, granola, and high-fat breads. Additionally, eating red meat was associated with an increased risk for chronic pancreatitis according to research findings.
Foods to Embrace in Your Pancreatitis Diet
While the list of foods to avoid might seem extensive, there are numerous delicious and nutritious options that support pancreatic health and provide essential nutrients.
Lean Proteins
Eating boneless chicken breasts and most fish helps keep your meals low in fat while providing high-quality protein necessary for tissue repair and immune function. Focus on cooking methods like baking, steaming, or grilling without added fats.
Excellent protein choices include:
- Skinless poultry (chicken, turkey)
- White fish (cod, halibut, tilapia)
- Egg whites
- Tofu and tempeh
- Low-fat dairy products (if tolerated)
Complex Carbohydrates
Unlike refined carbohydrates, complex carbs provide sustained energy without causing dramatic blood sugar spikes. Starchy vegetables, lean meats, and low-fiber vegetables and fruits form the foundation of a pancreatitis-friendly diet.
Recommended complex carbohydrates include:
- Brown rice and quinoa
- Sweet potatoes
- Oatmeal
- Whole grain pasta (in moderation)
- Bananas and other low-fiber fruits
Vegetables and Fruits
Fresh produce provides essential vitamins, minerals, and antioxidants while remaining naturally low in fat. However, some high-fiber vegetables might cause digestive discomfort during acute phases, so introduce them gradually.
Well-tolerated options typically include:
- Carrots
- Green beans
- Zucchini
- Spinach
- Applesauce
- Pears (peeled)
- Melons
Your Complete 7 Day Meal Plan for Pancreatitis
This carefully crafted meal plan provides balanced nutrition while respecting the dietary restrictions necessary for pancreatitis management. Each day includes three small meals and two snacks, totaling approximately 1,800-2,000 calories with less than 35 grams of fat.
Day 1: Gentle Start
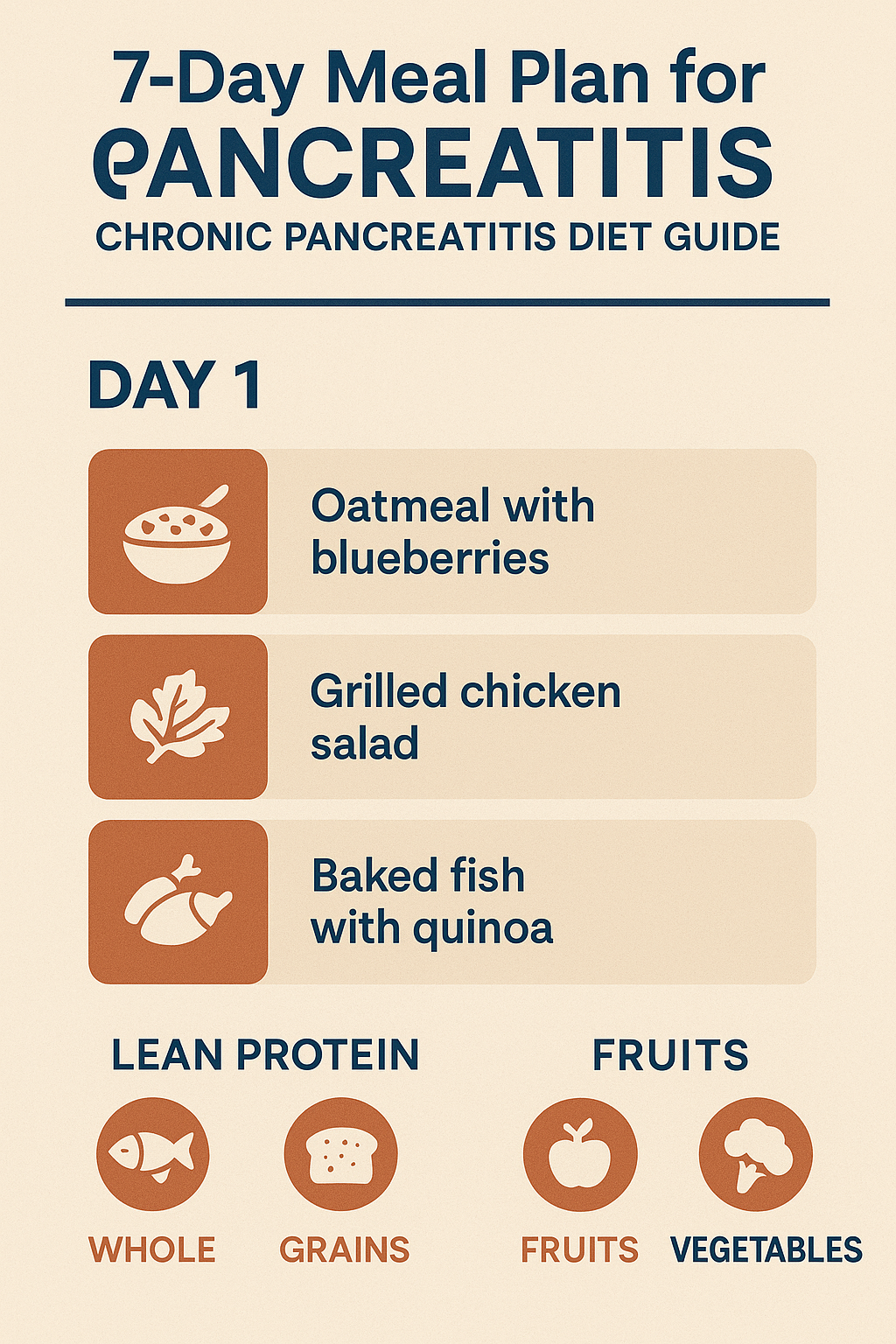
Breakfast:
- 1 cup oatmeal made with water
- 1/2 sliced banana
- 1 tablespoon honey
- Herbal tea
Mid-Morning Snack:
- 1 slice whole grain toast
- 2 tablespoons fat-free cream cheese
Lunch:
- 4 oz baked chicken breast (no skin)
- 1 cup steamed white rice
- 1/2 cup steamed carrots
- Water with lemon
Afternoon Snack:
- 1 medium apple (peeled)
- 6 oz fat-free yogurt
Dinner:
- 4 oz baked cod
- 1 medium baked sweet potato
- 1 cup steamed green beans
- Herbal tea
Day 2: Building Confidence
Breakfast:
- 2 egg whites scrambled (cooked with cooking spray)
- 1 slice whole grain toast
- 1/2 cup applesauce
- Water
Mid-Morning Snack:
- 1 rice cake
- 1 tablespoon almond butter (if tolerated)
Lunch:
- Turkey and vegetable soup (low-fat, low-sodium)
- 5 saltine crackers
- 1 small pear (peeled)
Afternoon Snack:
- 1/2 cup fat-free cottage cheese
- 1/4 cup canned peaches (in juice)
Dinner:
- 4 oz grilled chicken breast
- 1 cup quinoa
- 1/2 cup steamed zucchini
- Herbal tea
Day 3: Expanding Options
Breakfast:
- 1 cup rice cereal with fat-free milk
- 1/2 sliced banana
- Green tea
Mid-Morning Snack:
- 1 whole grain English muffin half
- 1 tablespoon sugar-free jam
Lunch:
- 4 oz baked tilapia
- 1 cup mashed potatoes (made with fat-free milk)
- 1/2 cup steamed spinach
Afternoon Snack:
- 1 medium orange
- 6 oz fat-free Greek yogurt
Dinner:
- 4 oz lean turkey breast
- 1 cup brown rice
- 1 cup steamed broccoli (small florets)
- Water with cucumber
Day 4: Midweek Motivation
Breakfast:
- 1 cup cream of wheat
- 1 tablespoon honey
- 1/2 cup berries (if tolerated)
- Herbal tea
Mid-Morning Snack:
- 2 rice cakes
- 1 tablespoon fat-free cream cheese
Lunch:
- Chicken and rice soup (homemade, low-fat)
- 1 small banana
- Water
Afternoon Snack:
- 1/2 cup applesauce
- 5 vanilla wafers (low-fat)
Dinner:
- 4 oz baked halibut
- 1 medium baked potato (no skin)
- 1/2 cup steamed asparagus
- Chamomile tea
Day 5: Staying Strong
Breakfast:
- 2 egg whites omelet with diced vegetables
- 1 slice whole grain toast
- 1/2 grapefruit
- Green tea
Mid-Morning Snack:
- 1 small apple (peeled)
- 6 oz fat-free yogurt
Lunch:
- 4 oz grilled chicken breast
- 1 cup white rice pilaf (fat-free)
- 1/2 cup steamed carrots
- Water with lemon
Afternoon Snack:
- 1 whole grain pretzel
- 1/4 cup hummus (if tolerated)
Dinner:
- 4 oz broiled sole
- 1 cup quinoa
- 1 cup steamed green beans
- Herbal tea
Day 6: Weekend Approach
Breakfast:
- 1 cup oatmeal
- 1 tablespoon maple syrup
- 1/2 cup melon
- Water
Mid-Morning Snack:
- 1 rice cake
- 2 tablespoons fat-free cream cheese
Lunch:
- Vegetable and barley soup
- 1 small roll (low-fat)
- 1 medium pear (peeled)
Afternoon Snack:
- 1/2 cup fat-free pudding
- 3 graham crackers (low-fat)
Dinner:
- 4 oz baked chicken breast
- 1 cup mashed sweet potatoes
- 1/2 cup steamed zucchini
- Mint tea
Day 7: Weekly Completion
Breakfast:
- 1 cup rice cereal
- Fat-free milk
- 1/2 sliced banana
- Herbal tea
Mid-Morning Snack:
- 1 whole grain toast
- 1 tablespoon sugar-free jam
Lunch:
- 4 oz poached salmon
- 1 cup brown rice
- 1/2 cup steamed spinach
- Water
Afternoon Snack:
- 1 medium orange
- 6 oz fat-free Greek yogurt
Dinner:
- 4 oz lean turkey breast
- 1 medium baked potato
- 1 cup steamed broccoli
- Chamomile tea
Meal Preparation Tips for Success
Successful implementation of your 7 day meal plan for chronic pancreatitis requires strategic preparation and cooking techniques that maximize nutrition while minimizing pancreatic stress.
Cooking Methods That Work
Flavor your foods with herbs and spices (such as basil, tarragon, or mint), fat-free sauces, or lemon juice instead of butter. This approach allows you to create flavorful meals without relying on high-fat ingredients that can trigger symptoms.
Recommended cooking methods include:
- Steaming vegetables to preserve nutrients
- Baking proteins without added fats
- Grilling with non-stick cooking spray
- Poaching fish in low-sodium broth
- Slow cooking tough cuts of lean meat
Kitchen Equipment Essentials
Investing in the right kitchen tools can significantly simplify meal preparation and help you stick to your pancreatitis diet long-term. Essential equipment includes:
- Non-stick cookware to minimize oil usage
- Steamer baskets for vegetables
- Digital food scale for portion control
- Fat separator for broths and soups
- High-quality blender for smoothies
Batch Cooking Strategies
Preparing larger quantities of staple foods can save time and ensure you always have appropriate meals available. Consider batch cooking:
- Brown rice and quinoa for the week
- Baked chicken breasts for multiple meals
- Vegetable soups in large quantities
- Hard-boiled egg whites for quick protein
Managing Symptoms and Adjusting Your Plan
Even with careful planning, you may experience symptom fluctuations that require temporary dietary modifications. Understanding how to adapt your 7 day meal plan for pancreatitis during different phases of your condition ensures consistent nutrition support.
During Acute Flare-ups
When experiencing increased pain or digestive symptoms, temporarily reduce your meal size and fat content even further. Focus on easily digestible foods like:
- Clear broths
- Plain white rice
- Banana
- Applesauce
- Herbal teas
Gradual Reintroduction
As symptoms improve, slowly reintroduce foods from your regular meal plan. Start with small portions and monitor your body's response before increasing quantities or adding new foods.
Working with Healthcare Providers
With the assistance of a healthcare provider or nutritionist, it's important to design a diet that excludes fat, alcohol, sugar, and processed foods. Regular consultations help ensure your meal plan meets your individual needs and adjusts to changes in your condition.
Nutritional Supplements and Enzyme Therapy
Many people with chronic pancreatitis require additional support beyond dietary modifications alone. Understanding when and how to incorporate supplements can significantly improve your nutritional status and symptom management.
Pancreatic Enzyme Replacement Therapy (PERT)
Most individuals with chronic pancreatitis benefit from prescription pancreatic enzymes taken with meals. If pancreatic enzymes are prescribed, it is important to take them regularly in order to prevent flare-ups. These enzymes help compensate for your pancreas's reduced ability to produce adequate digestive enzymes naturally.
Fat-Soluble Vitamin Supplementation
Due to malabsorption issues, many people with pancreatitis develop deficiencies in vitamins A, D, E, and K. Regular blood testing can identify deficiencies, and your healthcare provider may recommend specific supplements to address these gaps.
Medium-Chain Triglycerides (MCTs)
Some individuals find MCT oil helpful because these fats require less pancreatic enzyme activity for absorption. However, introduce MCTs gradually and under medical supervision, as tolerance varies significantly between individuals.
Lifestyle Factors That Support Your Meal Plan
Success with your 7 day meal plan for chronic pancreatitis extends beyond food choices. Several lifestyle factors can significantly impact your digestive health and overall well-being.
Stress Management
Chronic stress can exacerbate pancreatitis symptoms and interfere with digestion. Incorporating stress-reduction techniques such as meditation, gentle yoga, or deep breathing exercises can complement your dietary efforts.
Physical Activity
While intense exercise might be challenging during flare-ups, gentle movement like walking can promote digestion and overall health. Always consult your healthcare provider before starting any new exercise program.
Sleep Quality
Poor sleep can affect hormone production and digestive function. Prioritizing consistent sleep schedules and creating a restful environment supports your body's healing processes.
Long-term Success and Sustainability
Maintaining a restricted diet long-term requires strategies that prevent monotony and ensure nutritional adequacy. Here are approaches that have helped me and many others sustain healthy eating patterns over years.
Variety Within Restrictions
Even with limited food choices, you can create variety through different preparation methods, seasoning combinations, and meal timing. Experiment with herbs, spices, and fat-free sauces to prevent flavor fatigue.
Social Eating Strategies
Dining out and social gatherings can feel challenging when following a strict pancreatitis diet. Research restaurant menus in advance, communicate your needs clearly, and don't hesitate to make special requests. Many restaurants can accommodate dietary restrictions with advance notice.
Building Support Networks
Connecting with others who understand the challenges of living with pancreatitis can provide emotional support and practical tips. Online communities, local support groups, and working with experienced dietitians familiar with pancreatitis can make a significant difference in your long-term success.
Monitoring Progress and Making Adjustments
Your 7 day meal plan for chronic pancreatitis should evolve as your condition changes and as you learn more about your individual triggers and tolerances.
Symptom Tracking
Keeping a detailed food and symptom diary helps identify patterns and potential triggers. Note what you eat, when you eat, portion sizes, and any symptoms that occur. This information proves invaluable when working with healthcare providers to optimize your diet.
Regular Health Assessments
Schedule regular follow-ups with your healthcare team to monitor your nutritional status, pancreatic function, and overall health. Blood tests can identify nutritional deficiencies before they become symptomatic, allowing for proactive intervention.
Flexibility and Adaptation
Remember that managing chronic pancreatitis is an ongoing process. What works today might need adjustment tomorrow, and symptoms can vary based on stress, illness, or other factors. Maintain flexibility in your approach while staying committed to the core principles of pancreatitis nutrition.
The Path Forward: Hope and Healing
Living with chronic pancreatitis and following a restrictive diet isn't easy, but it is absolutely manageable with the right approach and support. This 7 day meal plan for pancreatitis provides a foundation for better symptom management and improved quality of life.
Remember that every small step toward better nutrition is progress worth celebrating. Some days will be more challenging than others, and that's completely normal. Focus on consistency rather than perfection, and don't hesitate to seek support when you need it.
The journey of managing pancreatitis through nutrition has taught me that food can be medicine when chosen and prepared thoughtfully. While the restrictions might feel overwhelming initially, many people find that their overall relationship with food improves as they become more mindful of how different foods affect their body.
Your health journey is unique, and this meal plan should serve as a starting point rather than a rigid prescription. Work closely with your healthcare team to personalize these recommendations based on your specific needs, preferences, and medical history.
With patience, dedication, and the right nutritional strategy, you can successfully manage your pancreatitis symptoms while maintaining good nutrition and enjoying satisfying meals. The path to better health starts with that first conscious food choice, and every meal is an opportunity to support your body's healing process.
Frequently Asked Questions (FAQ)
Q: How long should I follow a 7 day meal plan for pancreatitis?
A: A structured meal plan should be followed consistently, but it's not limited to just seven days. Use this 7 day meal plan for chronic pancreatitis as a template that you can repeat and modify based on your symptoms and tolerance. Most people with chronic pancreatitis need to follow dietary restrictions long-term, adjusting the plan as their condition changes.
Q: Can I drink alcohol while following a pancreatitis meal plan?
A: Alcohol should be completely avoided when managing pancreatitis, as it can trigger flare-ups and worsen pancreatic inflammation. This restriction is particularly important for those with chronic pancreatitis, as alcohol is a major risk factor for disease progression.
Q: What if I experience pain after eating foods from the meal plan?
A: If you experience pain after eating any food from your 7 day meal plan for pancreatitis, temporarily eliminate that food and consult your healthcare provider. Individual tolerances vary, and what works for others might not work for you. Keep a detailed food diary to identify potential triggers.
Q: How much fat can I eat per day with pancreatitis?
A: Most healthcare providers recommend limiting fat intake to 20-30 grams per day during acute phases and 30-40 grams during stable periods. However, this varies by individual and should be determined with your healthcare team. The fat should be spread throughout the day rather than consumed in large amounts at once.
Q: Can I exercise while following a pancreatitis diet?
A: Gentle exercise like walking is generally beneficial and can aid digestion. However, avoid intense physical activity during flare-ups. Always consult your healthcare provider before starting any exercise program, especially if you're experiencing active symptoms.
Q: Do I need to take pancreatic enzymes with every meal?
A: If your doctor has prescribed pancreatic enzyme replacement therapy (PERT), you typically need to take them with every meal and snack that contains fat, protein, or carbohydrates. Follow your healthcare provider's specific instructions regarding timing and dosage.
Q: What are the signs that my 7 day meal plan for chronic pancreatitis is working?
A: Positive signs include reduced abdominal pain, fewer digestive symptoms, improved bowel movements, stable weight, and better energy levels. It may take several weeks to see significant improvements, so be patient and consistent with your dietary changes.
Q: Can I eat out at restaurants while managing pancreatitis?
A: Yes, but it requires planning and communication. Research menus in advance, call restaurants to discuss your dietary needs, and don't hesitate to ask for modifications. Focus on grilled or baked proteins, steamed vegetables, and plain starches while avoiding sauces and fried foods.
Q: How do I prevent nutritional deficiencies on a restricted pancreatitis diet?
A: Work with a registered dietitian to ensure nutritional adequacy, consider vitamin supplementation (especially fat-soluble vitamins A, D, E, and K), and have regular blood tests to monitor nutritional status. Eat a variety of allowed foods to maximize nutrient intake.
Q: What should I do if I accidentally eat something high in fat?
A: If you accidentally consume high-fat foods, don't panic. Take your prescribed pancreatic enzymes if you have them, stay hydrated, and return to your regular meal plan with the next meal. Monitor symptoms and contact your healthcare provider if you experience severe pain or other concerning symptoms.


